Researchers emphasize the condition remains uncommon and say the findings aim to improve understanding, not alter vaccination guidance.
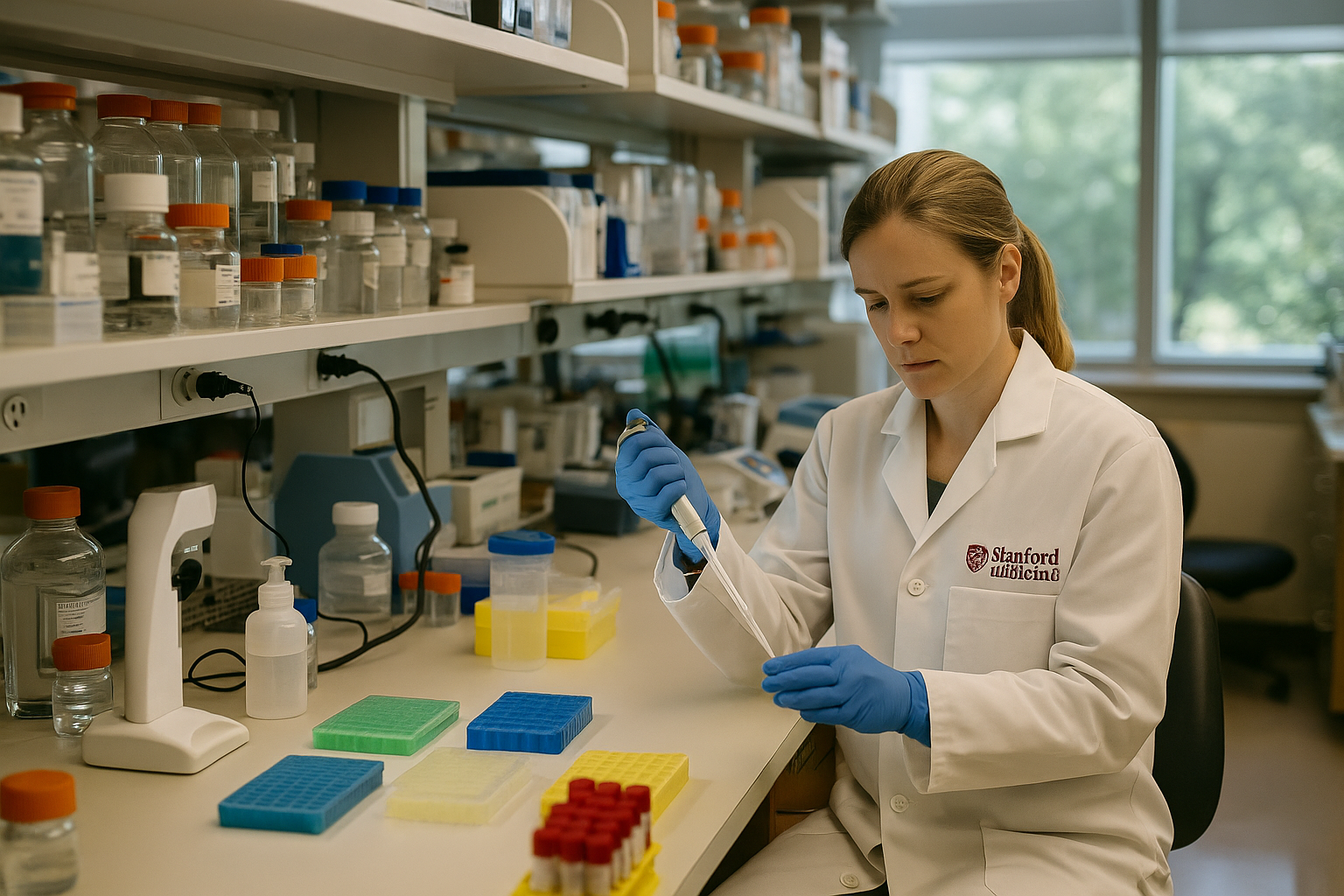
Stanford Medicine researchers have published a study exploring biological mechanisms that may help explain rare cases of myocarditis reported after mRNA COVID-19 vaccination, while stressing that the vaccines’ benefits continue to outweigh known risks.
A new study from Stanford Medicine examines why a small number of people have developed myocarditis after receiving mRNA-based COVID-19 vaccines. According to the researchers, the findings offer insight into possible biological mechanisms but do not establish a direct cause-and-effect relationship.
Myocarditis, an inflammation of the heart muscle, has been reported in rare instances following mRNA vaccination, particularly among younger males after a second dose. Public health agencies have consistently said these cases are uncommon and typically mild, with most patients recovering fully.
The Stanford researchers analyzed immune responses associated with mRNA vaccines and identified pathways that may contribute to inflammation in susceptible individuals. They said the study helps clarify how myocarditis might occur in rare cases, rather than determining how often it happens.
The authors emphasized that mRNA vaccines have been administered to hundreds of millions of people worldwide and have been shown to significantly reduce the risk of severe COVID-19, hospitalization, and death. They cautioned against interpreting the findings as evidence that the vaccines are unsafe.
Health experts note that COVID-19 infection itself carries a higher risk of myocarditis than vaccination. Regulatory agencies, including the CDC and FDA, continue to recommend mRNA vaccines for eligible populations based on extensive safety monitoring.
Stanford Medicine said the study could help guide future vaccine development and identify individuals who may be more susceptible to rare inflammatory responses. The findings have not prompted changes to current vaccination recommendations.